Whatever position one takes in the political battle over health care reform, all sides confront the same stubborn fact: the U.S. spends more than twice as much per capita on health care as other developed countries do—and yet fails to provide health coverage for all of its citizens.
Broader coverage is a social good, but the debate quickly becomes mired in matters of cost. At the current high levels of spending, can U.S. society afford to cover everyone? Meanwhile, estimates of excess or unnecessary costs in the U.S. health-care system have ranged as high as $750 billion per year. Depending on who’s talking, those excess costs are blamed on above-average doctors’ compensation, incentives that encourage clinicians to maximize the volume of procedures, high administrative costs associated with private insurance, unregulated prices for pharmaceuticals and medical products, and high malpractice costs, to name a few. As the debate rages on, the demand for health services increases.
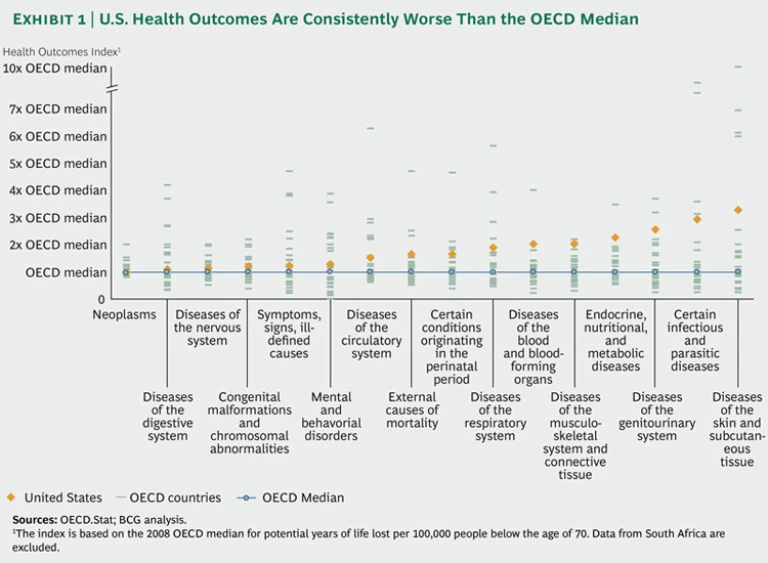
And yet, for all the focus on the high cost of health care, remarkably little attention is paid to what U.S. society is getting for its investment—that is, the actual health outcomes delivered by the U.S. health system. Most Americans would be shocked to learn that in nearly every disease group tracked by the 34 countries constituting the Organisation for Economic Co-operation and Development (OECD), U.S. health outcomes are worse—and sometimes considerably worse—than the OECD median. (See Exhibit 1.)
Those poor health outcomes are a human loss; they also represent enormous wasted economic value. We estimate that if the U.S. had been able to improve its health outcomes to the level of the 2008 OECD median (the most recent year of available comparable data), the result in 2011 would have been nearly 2.4 million statistical life-years saved. At standard rates used by health policy analysts for calculating the economic value of a statistical life-year (VSLY), that represents some $500 billion in potential economic value.
A Sustainable Approach to Health Reform
We believe that targeting better health outcomes is the key to sustainable health reform. Indeed, we think such a focus is the only way both to improve the quality of care and to curb excess health-care spending.
Putting the improvement of health outcomes at the center of health reform emphasizes the value that society is getting for its health care investment. It also has the benefit of engaging health care providers—not only clinicians but also medical-device makers and drug companies—in a positive approach to health care reform. Making value the centerpiece of changes in the health system has the potential to reorient clinical practice and incentives so that providers compete not on the basis of who delivers the most procedures or sells the most drugs (whether those procedures and drugs are actually linked to improved outcomes or not) but rather on the basis of who delivers the best value, understood as the best health outcomes for a given level of cost. What’s more, until U.S. society creates a more efficient value-based health-care system, it will never be able to rationally address the global cost question—that is, what is the “right” level of health care spending for all stakeholders, including patients and payers?
Seen from this perspective, the $500 billion figure can be understood as the potential return on investment in value-based health care. But how to get started in realizing that return? The answer lies in the data. The U.S. health system—patients, payers, providers, and suppliers—must join together in more deliberate and systematic tracking of health outcomes.
Outcomes Measurement: The Key to Value-Based Health Care
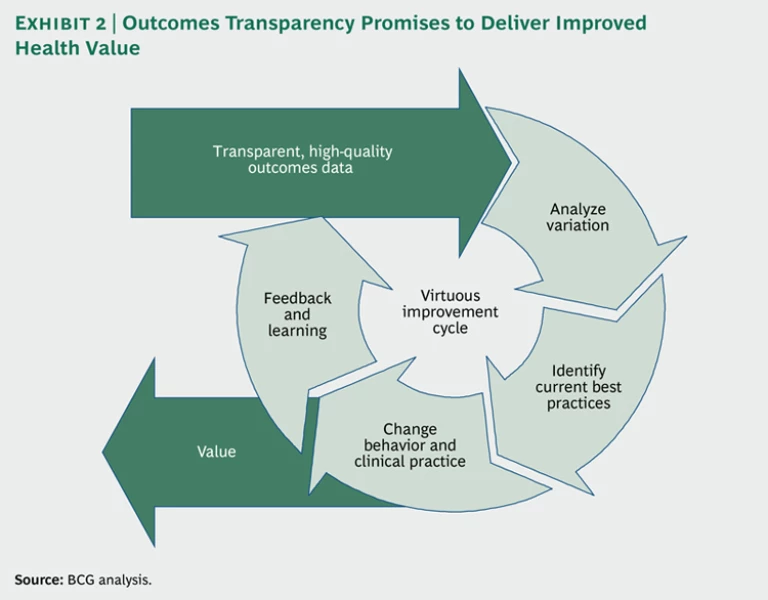
In the past few years, BCG has conducted extensive international research on national outcomes registries—databases that systematically capture information on outcomes for all or nearly all of the patients in a country, region, or network of clinical sites with regard to a particular disease, condition, or medical procedure. The critical finding of our research is that these data make it possible to identify variations in health outcomes across clinical sites, analyze the root causes of those variations, and codify best practices (that is, those that produce the highest-quality outcomes). Making the data and analysis transparent—in the first instance, to clinicians, and eventually also to the public at large—then becomes the catalyst for the definition of new standards, the dissemination of best practices across the system, reductions in outcomes variation, and improvements in median health outcomes over time. (See Exhibit 2.) In addition, systematic quality improvement of this type often has the positive side effect of lowering total health-care costs for some medical conditions and procedures, because unnecessary procedures are eliminated, expensive complications occur less frequently, and repeat treatments are avoided by “getting it right the first time.”
Although the U.S. has a number of excellent outcomes registries, the complexity and fragmentation of the U.S. health-care system has limited their spread. At the moment, there is no coordinated national system in U.S. health care for tracking health outcomes by clinical site.
What would be the potential economic impact of a comprehensive health-outcomes reporting system in the U.S.? The very lack of systematic outcomes data at the disease level makes such a calculation extremely difficult. Still, it is possible to put some broad parameters around the question.
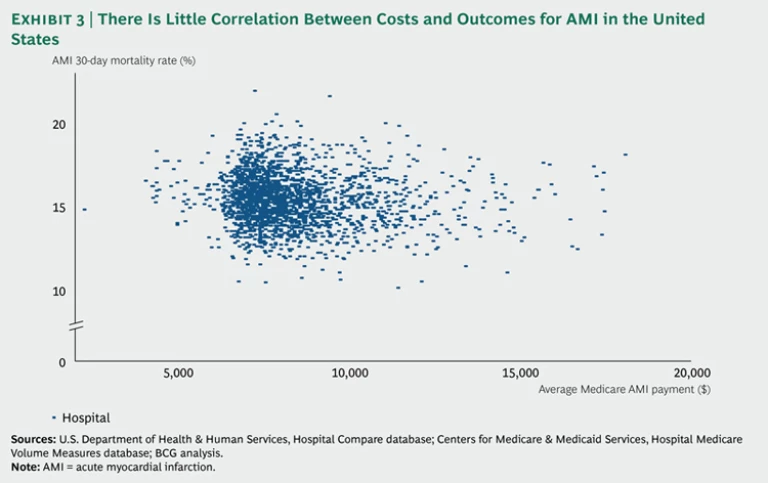
We know that there is tremendous variability in health care outcomes and health care costs across the U.S. health system. Both Medicare and the federal government’s Agency for Healthcare Research and Quality (AHRQ) have reported considerable variation in outcomes across regions and clinical sites.4 And the Dartmouth Atlas of Health Care has documented enormous variation in average Medicare spending per patient across U.S. health-referral regions.
One much-studied condition for which there are reasonably good data is acute myocardial infarction (AMI), or heart attack. Not only does the 30-day mortality rate for Medicare AMI patients vary widely by hospital, but there is little correlation between outcomes and costs. (See Exhibit 3.)
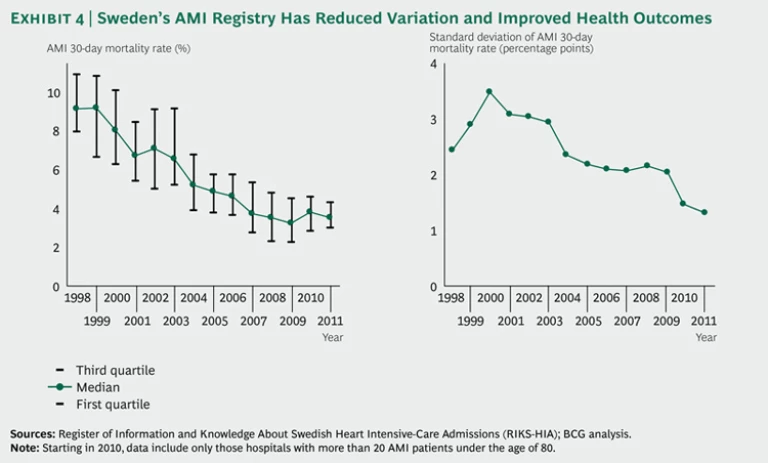
AMI is also one condition for which the existence of an outcomes registry has been shown to contribute to improvements in health outcomes. For example, the existence of a comprehensive AMI registry since 1998 in Sweden correlates with improvements in best practice and a continuous decline in that country’s 30-day AMI mortality rate. Although some inevitable variation across Swedish clinical sites still exists, the standard deviation has also narrowed considerably over time—from a high of 3.49 percentage points in 2000 to a low of 1.31 percentage points in 2011. (See Exhibit 4.) For comparison purposes, Sweden reduced its mean 30-day mortality rate by 62 percent from 2000 through 2008, compared with a reduction of only 26 percent in the U.S. during the same time period.
What would be the impact of similar improvements in the U.S.? We estimate that if the poorer-performing half of U.S. hospitals treating Medicare patients in 2011 had been able to achieve the 2009 U.S. median 30-day AMI mortality rate, the result would have been roughly 6,300 additional quality-adjusted statistical life-years, representing an economic value of $1.1 billion.
Additional value could also be expected in the form of costs avoided. For example, total Medicare spending on hospital-based AMI-related procedures was approximately $1.4 billion in 2008. In that year, if the more expensive half of U.S. hospitals had achieved the median cost per AMI admission, Medicare would have saved $146 million—about 11 percent of Medicare spending on AMI procedures. And if the poorer-performing half of U.S. hospitals had achieved the median AMI 30-day readmission rate, Medicare would have saved an additional $34 million in avoided readmission costs, another 2.5 percent of spending.
At first glance, these absolute dollar amounts may seem small. However, the diagnosis-related group (DRG) categories for AMI include patients receiving only diagnostic procedures (and therefore exclude angioplasty and bypass) and apply only to the hospital-related reimbursement for the condition—not to the total cost, including transportation, emergency-room charges, physician payments, additional diagnostics and procedures, and follow-up care. Nor do these DRG categories encompass the broader costs of treating the underlying disease. Thus, our analysis addresses only the tip of the iceberg—but even here we see considerable potential value in reducing variation and improving outcomes.
What might be the economic impact of extending such savings throughout the entire U.S. health-care system? For an order-of-magnitude estimate, consider that if Medicare spending in the country’s 306 health-referral regions that are currently above the median were reduced to the 2009 median, the result would be an 8 percent savings in total Medicare spending.
Introducing ICHOM
These numbers suggest the enormous potential economic benefit of a value-based approach to health care that serves to better align outcomes with costs. And focusing on improving health outcomes through the development and use of comprehensive health-outcomes data is an effective place to start. That is why BCG has partnered with Michael Porter’s Institute for Strategy and Competitiveness at Harvard Business School and with Sweden’s Karolinska Institute to create the International Consortium of Health Outcomes Measurement (ICHOM).
The mission of ICHOM is to serve as a catalyst for the global value-based transformation of health care by facilitating patient-outcome reporting and supporting the definition and dissemination of best practices. In providing a consolidated global source of outcome measures by medical condition, we hope to encourage transparency and international standardization.
Standardized metrics will allow clinicians to benchmark and assess comparative performance across care sites, document variations in health outcomes, identify best practices, and steer resources toward those interventions and practices that have the highest impact. They are also a requirement for payers and patients to be able to rank providers of a specific procedure and to shift to bundled payments that reimburse clinicians for the actual health impact achieved rather than for procedures performed.
It is not the goal of ICHOM to impose specific metrics on clinicians or to discourage innovation in the development of new and potentially more effective metrics. Rather, the goal is to serve as a forum for debate and international consensus-building. ICHOM will bring together the leading clinicians associated with outcomes registries for a given health condition to discuss the differences among the various metrics they have chosen and to agree upon a minimal set of metrics that will allow data sharing and comparison across registries and across global cohorts of patients.
ICHOM provides a necessary first step toward reorienting health care reform around more systematic reporting and tracking of outcomes for defined medical conditions and procedures. With this essential information in hand, core stakeholders will be better able to engage in a rational discussion about the appropriate level of spending to achieve a desired health-care outcome. We believe that this will lead to broader adoption of value-based health care in the U.S. and around the world—and, ultimately, to better health care for all.