Consider some sobering and little-known facts: Hepatitis C (HCV) is the most common and deadly infectious disease in the United States, beating out HIV, tuberculosis, and 57 other illnesses tracked by the Centers for Disease Control and Prevention (CDC). More than 4 million Americans are infected—most of them baby boomers (born between 1945 and 1965)—but only 50% have been diagnosed. The remainder are unaware that they have contracted the virus, thus putting themselves and others at risk. And while mortality rates for most infectious diseases are decreasing, deaths from HCV are rising over time. According to the CDC, nearly 20,000 deaths were reported in 2014, up from just 11,000 in 2003.
Perhaps worst of all is that although HCV is common and deadly, about 95% of the time it can be cured with antiviral treatments. Media attention has focused on the high cost of these therapies, but other roadblocks are even more problematic. For instance, there is a lack of awareness about the disease, its risk factors, and available treatments not only among patients and members of the general population—but also among nurses, physicians, and other health care providers.
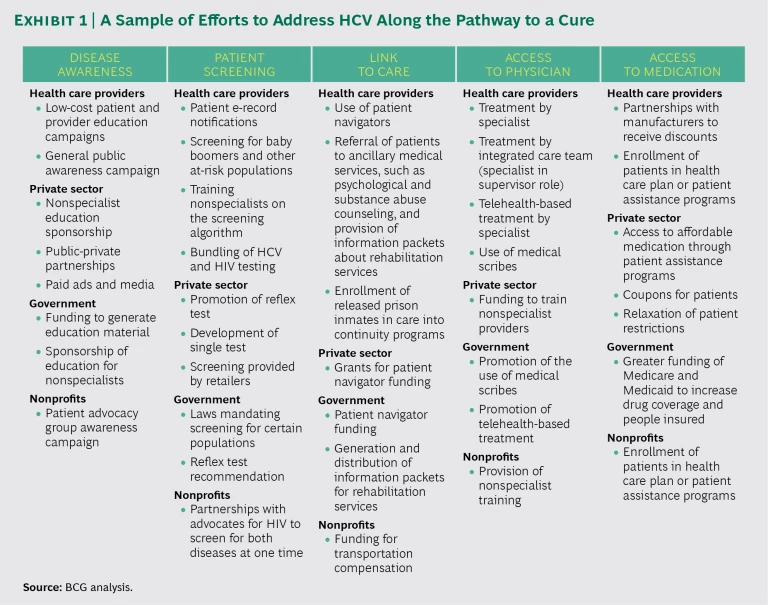
Current efforts to address HCV have found a measure of success. (See Exhibit 1.) However, they tend to be restricted to specific regions or patient populations. Complementing and building on these solutions will require a nationwide, integrated approach along each step of the “patient cascade”—the path that patients follow on their way to a cure. With adequate funding, the right incentives, and a strategic, coordinated effort by an array of stakeholders, HCV could be virtually eliminated in the US within a decade.
A Silent Killer
The three varieties of hepatitis—A, B, and C—are all spread by contact with contaminated blood and affect the liver, but they are caused by different viruses. Vaccines protect only against types A and B. Of individuals who contract the C virus, 75% to 85% develop chronic hepatitis C. It is estimated that baby boomers are three times more likely than the general population to become infected with HCV, likely because of contamination during medical procedures and injection drug use.
Because most people experience no symptoms during the early stages of the disease, it can progress undetected for many years, leading to cirrhosis, liver cancer, and liver failure. But if diagnosed and treated early on, patients usually recover fully. Unfortunately, this is not the case for most patients. How can we address the problem and eliminate this deadly disease in the US?
Taking Action Toward Elimination
To find out, The Boston Consulting Group conducted a thorough analysis of HCV research and literature, interviewed leading experts, and evaluated existing treatment models. We identified seven critical actions that must be taken to eliminate HCV in the United States.
Increase awareness in the general public. HCV is not as well publicized as other major infectious diseases, largely because it receives less funding. For instance, HCV gets only about 2% of the funding to increase public awareness that HIV and AIDS receive. Other key components of an effective campaign are missing as well, such as celebrity spokespersons and educational efforts that target specific patient populations: rural or urban, insured or uninsured, older or younger. As a result, most people are unaware of how common and deadly HCV is and what its risk factors are.
According to our estimates, increasing awareness would require an investment of about $400 million over the next five to ten years. This is a large number, but stakeholders—such as hospitals, pharmaceutical companies, and the government—have economic incentives to fund these efforts.
Educate health care providers. Because many health care providers have limited knowledge of HCV’s risk factors, they miss opportunities to identify and screen high-risk individuals. A recent survey showed that up to 20% of primary care physicians (PCPs) failed to identify baby boomers as high risk. Furthermore, up to 75% of physicians failed to identify other risk factors, such as blood transfusions prior to 1992, intravenous drug use, alcohol abuse, multiple sex partners, and patients undergoing hemodialysis. In another survey, almost 40% of PCPs believed—incorrectly—that HCV is still treated primarily with injections of interferon. Only 35% knew that the new HCV therapies are highly effective.
Equipping the medical profession with the needed training and knowledge would require fielding a full-time team of 60 to 100 medical educators over the next several years.
Increase screening of at-risk populations. Even when at-risk people are aware of HCV, they may not be tested for the virus. Sometimes this is because they lack information on where to get tested or because they do not want to incur the associated costs. What’s more, because of the stigma associated with the disease, few people in the general population get screened unless prompted by their PCPs. And some people—especially heavy drug users and those with low incomes—simply don’t get regular medical attention.
More knowledgeable medical providers and better outreach efforts can increase screening rates. Retail pharmacies are also well positioned to screen patients and refer them to follow-up resources. In-store screening centers could provide a valuable community service while generating new sources of income. Another promising approach is to set up social businesses, ventures whose main objective is to address a social problem—in this case, the low rates of screening among at-risk populations. (See “The Value of Social Business,” BCG article, October 2014.) For instance, community screening centers could be established, where some or all of the profits from screening or related prescriptions could be used to fund HCV awareness campaigns within the community.
Simplify testing procedures. Currently, two different blood tests, performed on separate days, are required to obtain the most accurate diagnosis. The first test is for HCV antibodies; the second is for the virus itself. The CDC estimates that 51% of patients with a positive first test fail to show up for the second test, often because of the stigma associated with a positive diagnosis, an absence of symptoms, or lack of education about the disease.
Faster, simpler screening methods, such as one-step reflex testing, already exist and should be used more. Investments in companies that are innovating in this area should be encouraged as well.
Improve patient follow-up and access to care. Research shows that about 40% of patients who test positive for HCV fail to see a provider who is trained to treat the disease—in part because of a shortage of such providers. Moreover, many patients are not effectively educated and counseled on the disease’s progression, available treatments, and how to navigate available care. In some cases, patients are reluctant to make the necessary lifestyle changes, such as abstaining from alcohol or drugs. In addition, getting care is not as simple as a trip to the doctor for a prescription. Patients must make several visits to learn about the disease, be assessed for treatment, and get a treatment schedule. A liver biopsy is sometimes needed. Adding to the complexity is the need to navigate health insurance requirements or patient assistance programs or both.
Patient navigators, who help connect patients with HCV specialists and treatments, could help. We estimate that 1,500 to 2,000 such navigators, linked to screening hospitals and providers, would be needed.
Increase the number and reach of qualified physicians. Even when patients are motivated to seek treatment, they may have difficulty finding a trained provider if they are not near a large, urban medical center. Appointment backlogs may also be dauntingly long—up to 6 months in some areas. The US has only about 27,000 doctors specializing in infectious diseases and hepatology, compared with more than 200,000 internists and PCPs.
By our estimates, the number of physicians trained to treat HCV would have to quadruple in order to handle the expected increase in patients. Using telehealth and medical scribes, who take notes during doctor appointments and enter information into the provider’s computer system, could improve efficiency and allow doctors to see greater numbers of patients in broader geographic areas. Training nonspecialists to diagnose and treat HCV could also help close the care gap—especially in parts of the country where health resources are scarce. A recent study showed that PCPs with just three hours of training can gain the skills needed to diagnose and treat most HCV patients.
Make treatment more financially accessible. Sometimes insurance will not cover a patient’s HCV treatments unless certain conditions are met; circumstances vary by state and type of plan. A number of these conditions, such as giving up alcohol and drugs, are within the patient’s control—but others are not. For instance, 25 states require that patients have a high degree of liver fibrosis (scarring caused by HCV), 6 states require a liver biopsy, and 30 states require that patients see a specialist only, not a qualified and trained PCP. Another obstacle is the cost of treatment. A typical 12-week regimen costs anywhere from $45,000 to $95,000, depending on the availability of rebates offered by pharmaceutical companies and the degree of fi-
nancial assistance a patient gets. While this is cost-effective for the health care system in the long run, it is still an expensive near-term cost for both patients and payers.
Despite these challenges, more than half of HCV patients have access to care today, whether through insurance, government programs, or patient assistance programs. Though we do see increased competition in the HCV drug market starting to drive down price, more work must be done to ensure that every patient has such access. Well-trained patient advocates are needed to help people get the financial support they are entitled to and navigate the often complex requirements for insurance and patient assistance programs.
A Strategic, Coordinated Effort
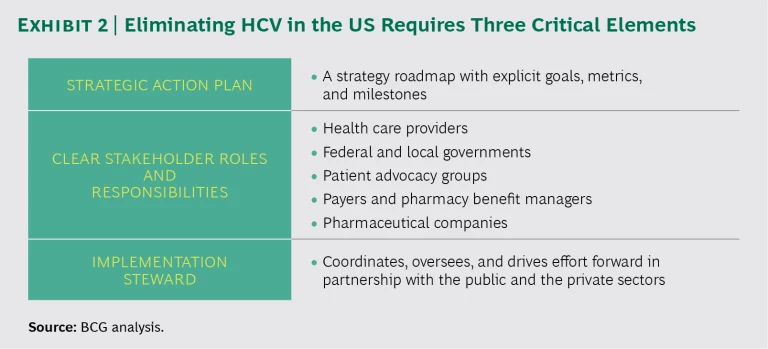
To succeed, these actions must be part of a nationwide, coordinated effort with three critical elements: a strategic action plan, clear stakeholder roles and responsibilities, and an implementation steward to orchestrate the effort. (See Exhibit 2.)
Strategic Action Plan. Given the wide variety of barriers, stakeholders, and potential solutions, a detailed strategy and roadmap to coordinate the effort is critical to success. The strategy must consider the differences among HCV patients and the fact that no single approach will work for everyone. Segmenting patients according to factors such as where they live (urban, suburban, or rural), what type of health care they have access to (large medical system, specialists, small practice, no access), and what other chronic conditions they may have is a necessary step toward tailoring the best solutions.
If ten years is the goal for elimination, then the roadmap must define clear interim objectives, metrics, milestones, and stakeholder responsibilities. Explicit deadlines and accountability will ensure that collaboration drives action and delivers results. Also critical is a process for monitoring progress, including an annual meeting to review key metrics and celebrate successes. Progress will be achieved and accelerated only through the partnership and commitment of key stakeholders.
Clear Stakeholder Roles and Responsibilities. At a minimum, five key stakeholders must work together to make sure that solutions are effectively funded and delivered. Each stakeholder has a critical role to play:
- Health care providers must identify, educate, screen, and treat more at-risk patients. PCPs and nurse practitioners are often the first line of defense against HCV. They can make an enormous difference by flagging at-risk individuals; connecting patients to screening and treatment resources, HCV specialists, and counseling services; and educating patients about the treatment options and care that go along with a positive diagnosis. Care providers can also take the lead in setting aggressive targets to eliminate HCV within their local populations, one community at a time. For example, electronic medical records can be programmed to flag patients that need HCV testing—a relatively simple intervention that has been shown to increase testing rates by up to 70% in a community hospital setting.
- Federal and local governments can support public awareness and treatment through legislation, grants, and funding for programs that provide education, medication, and other services to HCV patients. The federal government could also improve access to effective treatments by increasing funding for Medicare and Medicaid, licensing drugs for use by at-risk populations, and issuing state bonds. Sponsored workshops and training materials for health care providers and nonspecialists about best practices could also improve awareness and patient outcomes. New York is at the vanguard of increasing HCV awareness: in 2014, the state passed legislation requiring that every baby boomer who receives health services be offered testing for HCV.
- Patient advocacy groups can drive awareness efforts, lobby for funding, provide outreach and education to at-risk populations, and help those who test positive get access to care. These groups can also partner with providers and retail pharmacies to hold screening drives for at-risk populations that may not receive regular health care. Other areas of advocacy include establishing funding for telehealth and medical scribes, working to reduce insurance restrictions on treatment coverage, and helping patients navigate through assistance programs.
- Payers and pharmacy benefit managers (PBMs) can work to ensure greater access to treatment by going beyond simply negotiating with pharmaceutical companies to purchase HCV medicines at the lowest possible price. One option is to explore new financing mechanisms, such as special bonds that allow one or more payers to purchase HCV therapies over time, without delaying treatment. PBMs can help to ensure that any rebates from pharmaceutical companies directly benefit patients when possible.
- Pharmaceutical companies can continue supporting patients in four key ways: by using traditional advertising and social media to increase awareness; by funding patient assistance programs for those most in need; by making sure that patients can access these programs with minimal guidance; and by ensuring that the public understands how the value of HCV therapies warrants the cost—not just to patients, but to the health care system and society as a whole.
Implementation Steward. We strongly recommend this new, pivotal role to help orchestrate HCV elimination efforts across the US. The organization most likely to play this role would be a nonprofit or government entity that is already working to eliminate HCV. The implementation steward would coordinate, oversee, and drive these efforts forward, working closely with other groups and agencies and seeking ways to partner with the private and the public sectors to increase funding.
Hurdles remain despite the progress in addressing HCV. But with strong, visionary leadership, a coordinated strategy, and the commitment and collaboration of all stakeholders, the battle against HCV in the US can be won—and the disease completely eradicated.