It’s a $60 billion problem for health care providers every year—and that’s accounting only for nurses.
Health care systems throughout the US are grappling with workforce talent challenges, especially high attrition rates for clinical talent, which have big implications for both costs and care. At-risk jobs include registered nurses (15% to 25% attrition), technicians (20% to 25%), medical assistants (more than 30%), and home health aides (more than 60%). Since 2021, health care executives have cited these workforce challenges as their top issue in annual surveys conducted by the American College of Healthcare Executives (ACHE). Given an average attrition rate of 15% among the 4 million nurses in the US, we estimate the price tag for providers of hiring, bringing onboard, and training new nurses at about $60 billion a year.
Talent shortages and the related costs exacerbate the existential financial issues facing US health systems. Strong clinical-workforce programming that effectively addresses the needs of employees can significantly reduce turnover. Putting in place the processes that bring this strategy to life saves money and unlocks significant value—as much as 5% to 10% of clinical-labor costs, as well as improved patient outcomes.
Crafting an effective talent strategy also is essential to continuing to deliver world-class care. Below, we look at why people leave—and stay—and offer steps that any provider can take to reduce attrition, generate value for the organization, and improve the employee and patient experience.
Understanding Why People Leave
Clinical staff cite multiple reasons for quitting their jobs, with factors often including:
- Burnout and stress driven by understaffing and a taxing workload
- Dissatisfaction with managers stemming from a lack of effective frontline leadership development
- Financial rewards that are not commensurate with the physical and emotional exhaustion associated with the role
- A taxing administrative burden
- Limited career growth opportunities
A recent BCG survey of almost 700 nurses at health systems across the US revealed that the attrition risk for nurses is significantly higher than for people in other sectors and jobs (such as office employees). More than half of nurses (56%) say they are considering leaving their job. But there’s also good news for employers: nurses are 55% less likely to be looking for a new position if they enjoy their current one.
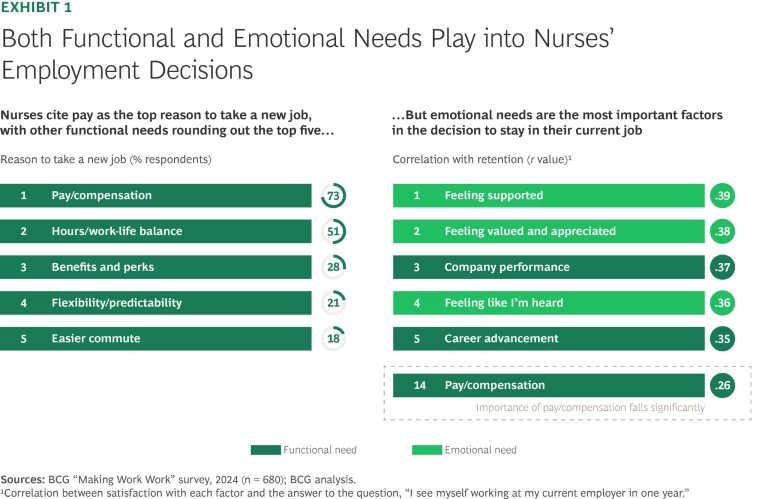
Not surprisingly, compensation is the most cited factor for people who are planning to leave a job and are evaluating other roles. Work-life balance is also extremely important. But when we examined why nurses remain in their roles, emotional factors—including feeling supported, valued, appreciated, and heard—are the most important criteria that influence them to stay. (See Exhibit 1.)
Differentiating the Workforce
To keep and develop talent, providers need to take a customer-centric approach to supporting their employees. This includes identifying how staff needs vary across distinct segments of the workforce. Employers that go beyond demographic and job-related information to better understand employees’ needs and characteristics can use existing data (such as surveys and statistics on patient outcomes) to identify the employees that need more attention and the actions that can help retain talent. Hospital- or regional-level data can be used to pinpoint pockets of success and highlight processes that can be replicated and scaled across larger systems.
Stay ahead with BCG insights on the health care industry
When we asked nurses about their job satisfaction and whether they intend to remain with their current employer and for how long, three employee segments emerged: lifers, launchers, and leavers. These are a useful starting point for understanding nurses’ needs.
- Lifers make up about 40% of the nursing workforce and are typically well on in their careers, with more than ten years of tenure. These employees feel a stronger sense of control over their time and workload than their less experienced colleagues. They are content with their roles and expect to remain with their current employer for the long term. They value recognition for their contributions and the opportunity to be the best they can be at their jobs.
- Launchers represent approximately 45% of the workforce. They are often under age 35, typically with three to ten years on the job, and they are eager to take the next step in their careers. These employees see their current role as a springboard to broader opportunities, whether at the current organization or elsewhere.
- Leavers account for about 15% of the workforce. They have typically been longest in the field, with tenure of ten years or more. They tend to feel a lack of fulfillment or motivation in their roles and are actively seeking new opportunities that offer more value, support, and alignment with their needs.
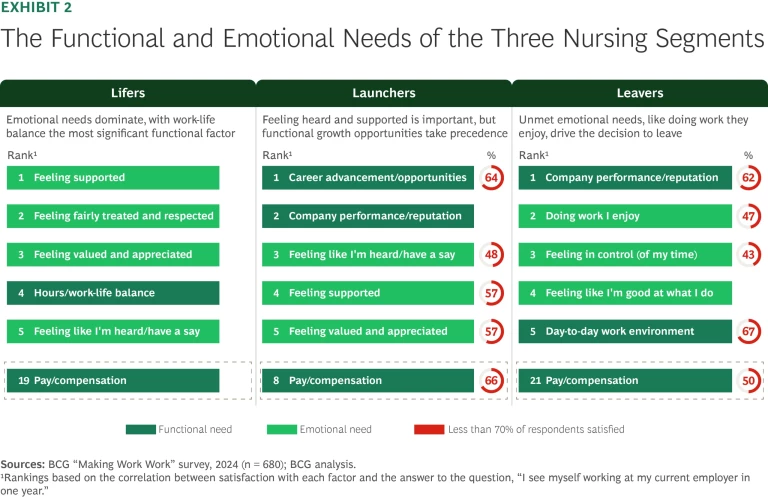
Nurses in each of these segments have their own functional and emotional needs, which can help in identifying the types of interventions that will have greatest impact. (See Exhibit 2.) Emotional needs dominate the list for lifers, with work-life balance being the most significant functional factor. While launchers care about feeling heard and supported, growth opportunities, such as career advancement, are even more important to them. Leavers have unmet needs (job enjoyment is a big one), and poor workplace conditions often drive their decision to leave.
Empower Employees
To meet employees’ differing needs, providers can do more to tailor programs or offerings to individual cohorts. For example, instead of optimizing for operational priorities—such as shift coverage, license and skill mix, and quality and regulatory compliance—they can offer more job and program flexibility, so staff have some freedom in scheduling, in selecting a mix of clinical practices, and in choosing whether to work in an acute or ambulatory setting. Such flexibility can make a difference, particularly for potential leavers who are seeking opportunities more in line with their needs and aspirations.
Flexibility and more career options allow employees to take charge of their professional development. Two important ways to facilitate employee choice are being transparent about the skills and responsibilities of different career paths and providing data about the choices that employees with similar skills have made. Providers can provide access to staff in roles about which employees may be interested. Such steps help equip people with the information they need to make informed choices about their future—and can be particularly helpful for launchers, who may otherwise think of leaving for another provider.
Health systems can also bolster internal mobility pathways into essential clinical roles. For instance, they can develop programs that give employees working in nonclinical areas the support they need to undertake the training required to move into patient care assistance and nursing positions.
Mentors are often powerful enablers of career advancement, and providers can make mentorship even more effective. Only 43% of nurses in our survey said that their managers help them plan for their careers in the long term. At the same time, they ranked mentorship as their second most enjoyable task overall. Mentorship programs can support both launchers looking for advice on next steps and lifers who want to be recognized for their experience and skill.
Following the pandemic, one health system recognized that being a nurse trainee or a relatively inexperienced nurse can be a lonely and scary experience, especially on night and weekend shifts. Management implemented a nationally recognized program for nurse mentors that provides peer coaches and takes the pressure off nurse managers who are managing large numbers of staff.
Take a Comprehensive Approach
To ensure that workforce retention strategies address the actual problems that employees face, leaders should include relevant employees in the development of solutions. For example, management can work with HR to design incentives and rewards for participation, but unless nursing leaders are asked to develop schedules that enable staff to participate, the programs will struggle to reach their intended scale. Designing retention programs in cooperation with in-house nurse leadership groups has proven to have a powerful impact.
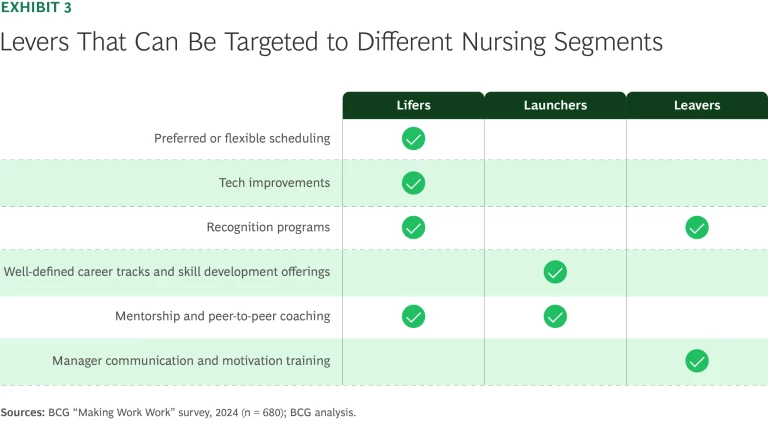
In a similar vein, nobody will object to a pay raise, but our research shows that pay alone only goes so far. Employers need to be more strategic in determining which levers will make the biggest difference for the employees they are trying to retain. (See Exhibit 3.) A co-creation and testing approach, which could include conducting regular follow-up surveys and publicizing the actions taken in response, helps to ensure that programs address employees’ needs.
Consider the case of a large health system that was experiencing widespread clinical-workforce challenges, particularly in nursing. Management took the following steps to reverse the unfavorable retention trends in ways that were consistent with the institution’s broader priorities:
- Establishing a clinical ladder that rewarded nurses and encouraged development while also focusing time and resources on evidence-based practices critical to patient care
- Formalizing pathways that gave nurses exploring other options an opportunity to continue contributing to the organization instead of moving on
- Developing frontline leadership programs that improved training while building a pipeline to supervisor roles that had been difficult to fill
- Creating pathways into nursing that offered hospital workers economic mobility while filling some of the most challenging vacancies at the hospital
Because these programs were designed with both the needs of nurses and the priorities of the health system in mind, the expected value is about 5% of the provider’s total spending on its nursing workforce, primarily by reducing its nursing attrition rate, which has been 15% to 20%.
Think Long Term
Talent development and retention are challenges that need continuing attention. Talent programs often fail when they are not set up with the infrastructure, resources, and change management processes that can provide support well into the future. Building in flexibility is critical to regularly refreshing offerings as needs change. Employees need to understand the value of career development programs and how they will pay off long term. Management should establish objective measurement systems, including both long-term engagement and attrition KPIs and leading indicators, to rigorously track progress. Other relevant measures include time to fill critical roles, turnover rates in key roles, and employee engagement and satisfaction scores. Leaders should also avoid overcommitting to staff at the outset, instead building credibility over time with successful execution and internal publicizing of new options and results.
Attrition is expensive and undermines quality of care and financial health. Providers that listen to their employees and take the right steps to address job satisfaction and retention rates will both save money and improve care. Moreover, smart talent strategies and a strong talent ecosystem will support the efforts of health systems to increase the efficiency and effectiveness of their overall operating models—and sustain those improvements for the long term.






