As the global population ages, many economies are bracing for a one-two punch: a shrinking workforce colliding with rising health and social care costs—the so-called “gray wave.” Healthy aging holds the potential not just to offset these impacts, but to add trillions in economic value by keeping people active, productive, and independent longer. What do we mean by healthy aging? The World Health Organization defines it as “the process of developing and maintaining the functional ability that enables wellbeing in older age.”
The benefits of healthy aging aren’t just economic, they’re personal. A longer life in good health means more time spent doing the things we value, from traveling and connecting with family and friends to contributing to our communities. BCG’s Global Study on Longevity, conducted for the St. Moritz Longevity Forum, surveyed 9,350 respondents across 19 countries. The study confirms that this vision of enjoying a long, healthy, satisfying life resonates with people from all backgrounds across the globe, even if they’re unsure how to achieve it.
As lifespans rise and science unlocks new ways to extend vitality, most people don’t start thinking about aging well until it’s too late. We call this the longevity paradox.
Longevity Is Built on Health Ambitions
In addition to confirming people’s desire to experience healthy aging, our survey also reveals something deeper: people are just as focused on the inputs—what they think they should do—as they are on the outcomes they hope to achieve.
Top of mind for most people is maintaining physical health and functional ability (29% cited this as their first priority), followed by eating a nutritious diet (25%), engaging in regular physical activity (22%), and getting quality sleep (22%). But close behind these are more emotional and existential goals: living with purpose and joy (22%) and staying mentally and creatively stimulated (19%).
The takeaway? People often confuse the outcomes of healthy aging (joy, purpose, functional ability) with the means by which we can make it happen (better diet, exercise, sleep). That confusion matters. Overemphasizing the means can feel like a stream of self-improvement homework, which rarely inspires lasting change in people. But anchoring the conversation in what people want—whether it’s dancing at their grandchild’s wedding or hiking into their 80s—is far more motivating.
This is where the idea of health ambitions comes in: the deeply personal goals that define what healthy aging looks like for each individual. Understanding these ambitions—and designing personalized communications, interventions, and technologies around them—may be the key to shifting behavior at scale. Because everyone’s health ambitions and the age when they begin taking action to achieve them are different, a one-size-fits-all approach won’t work. Motivation lives in the why, and personalization is how we reach it.
Our Starting Point—Too Little, Too Late
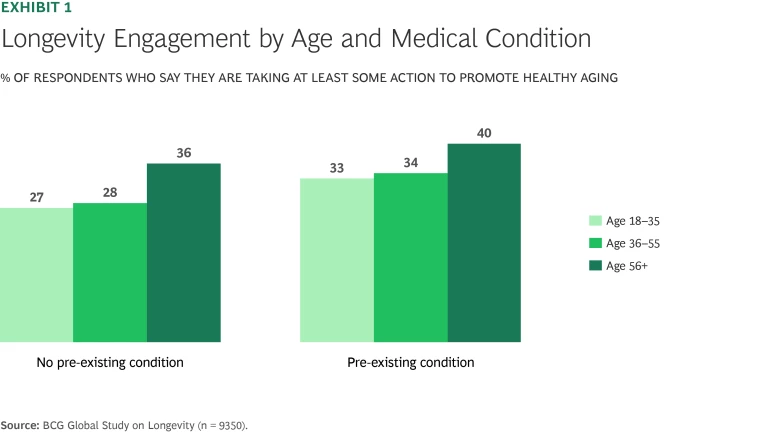
So where do people stand today on the path to healthy aging? Our research shows that most aren’t taking consistent action to support their long-term health, particularly when they’re still young and feel healthy. Even among the cohort of respondents aged 56 and older with pre-existing conditions, only 40% say they are taking active steps towards healthy aging. (See Exhibit 1.)
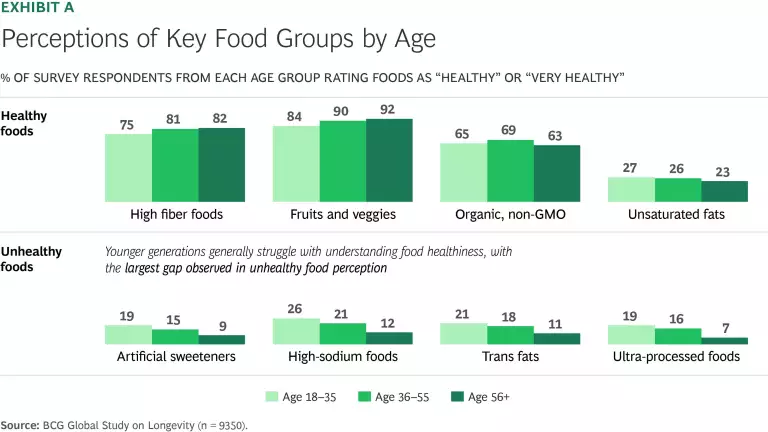
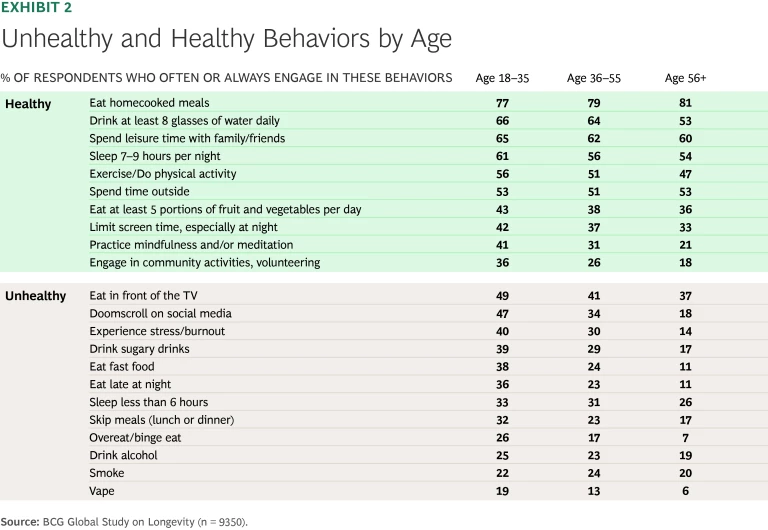
But the picture is more complex than simple disengagement. Younger generations, for instance, show high levels of both interest and inconsistency. They’re more likely than older cohorts to experiment with wellness trends and use health-tracking technology, but are also more likely to doomscroll, skip meals, or regularly down sugary drinks. The number of young people who report feeling stress/burnout (40%) is twice that of older generations. Young people are also the least informed about healthy dietary choices. (See “Food Perceptions, Behaviors, and Tackling the Obesity Epidemic.”)
Food Perceptions, Behaviors, and Tackling the Obesity Epidemic
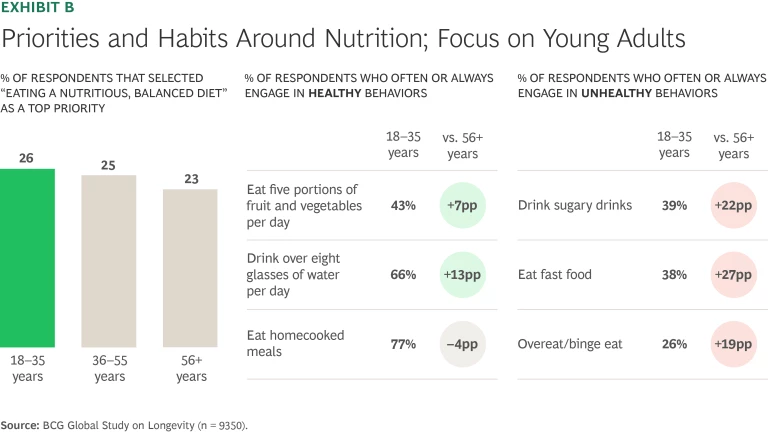
Education is only part of the solution. Younger generations, while appearing less informed, are more likely to engage in both the healthiest and unhealthiest nutrition-related habits. (See Exhibit B.)
Even among those who are well-informed, a majority across all age groups fail to eat balanced, nutritious meals, get enough vegetables, or drink the recommended eight glasses of water a day.
The need to take action is clear. With only half of adults exercising regularly, and even fewer following a healthy diet, the rise in obesity rates in many countries is unsurprising. To make progress, digital innovators, companies, and policymakers each have a role to play.
Digital platforms are taking a personalized, gamified approach to driving lasting behavior change. Noom, a personalized weight management and health app, delivers daily, tailored content to encourage changes in diet, exercise, and mindfulness. Through continuous testing and rapid feedback loops, Noom refines its messaging based on user responses and behaviors—helping 40% of users who remain engaged for at least four weeks lose 5% or more of their body weight. Noom’s personalization engine adapts to individual learning styles and preferences, with optional human coaches providing additional support.
Pharmaceutical companies are also drawing inspiration from digital platforms, launching direct-to-patient (DTP) platforms to address pain points in the patient journey. Platforms such as LillyDirect and NovoCare help improve access and affordability issues for GLP-1 medications that have proven successful in promoting weight loss, offering deeply discounted cash-pay pricing for patients whose insurance does not cover these products. While costs to patients remain a barrier, these initiatives have expanded reach and sparked a broader trend in the US to explore using DTP platforms to solve unmet health communication needs.
The numbers are similarly discomforting across the population. Fewer than half of respondents in any age group consistently engage in foundational healthy behaviors, like exercising, eating well, or getting enough sleep. (See Exhibit 2.)
And yet, the upside for people making even modest changes is enormous. A recent analysis by the US Department of Veterans Affairs found that choosing the healthier option across just eight behaviors—such as regular physical activity, eating a plant-based diet, quality sleep, and avoiding substance misuse—was associated with up to 24 extra years of life.
The Five-Step Ladder of Longevity Engagement
Our survey data underscores that people’s approach to healthy aging isn’t uniform. Interest and intention don’t always translate into action. And in a landscape flooded with conflicting advice, social media influence, and unfiltered information, it’s not always clear where to start. The goal is to help people move from passive awareness to proactive, personalized care.
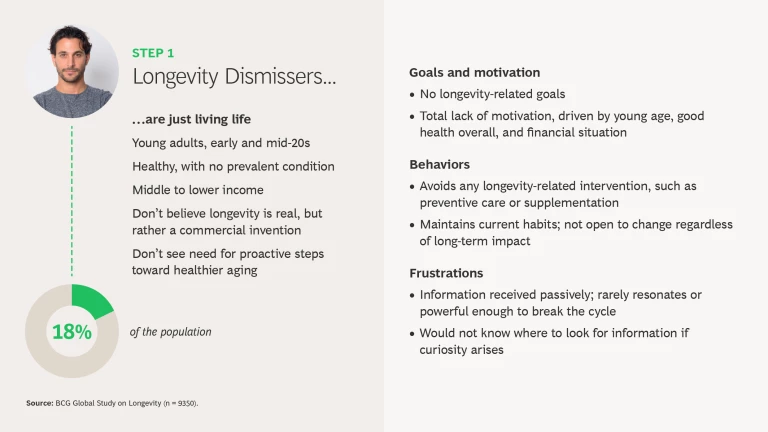
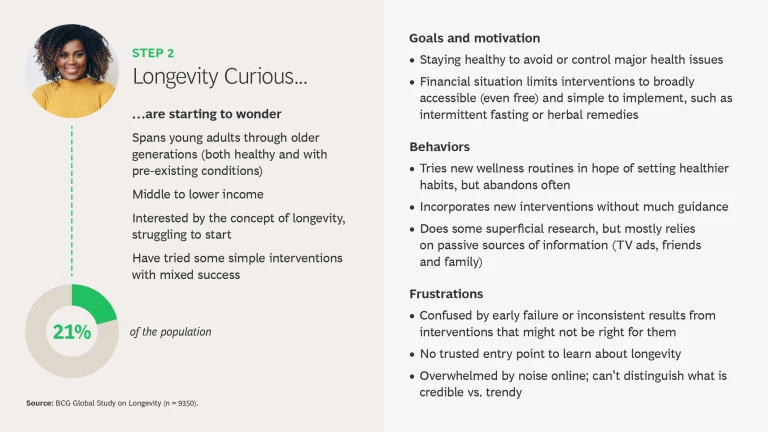
To understand the progression towards healthier aging, we used our survey data to map the five stages of engagement people currently have with longevity-based behaviors—and clear personas emerge. People differ in the actions they are taking at each stage as well as the sources they turn to for information and advice. (See “The Longevity Engagement Ladder” slideshow and Exhibit 3.)
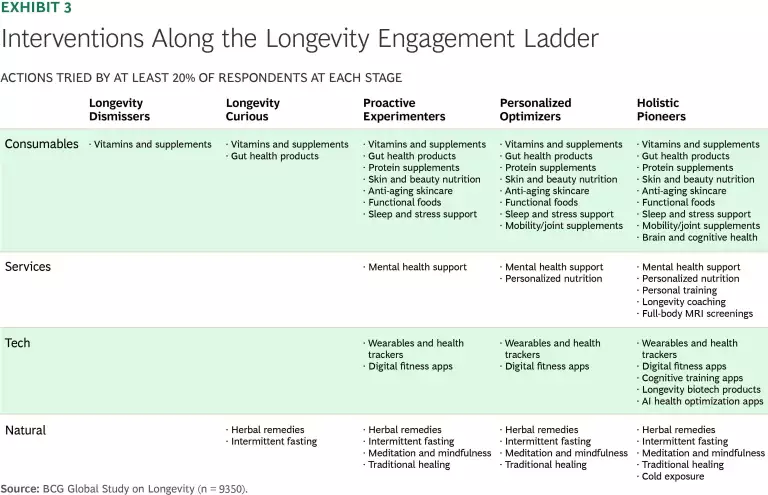
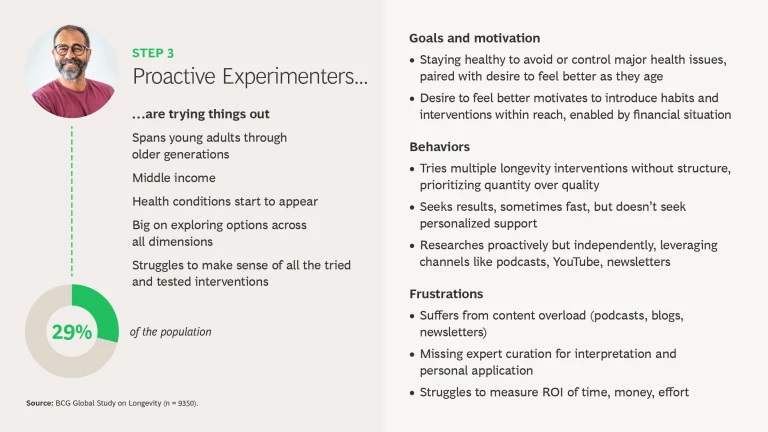
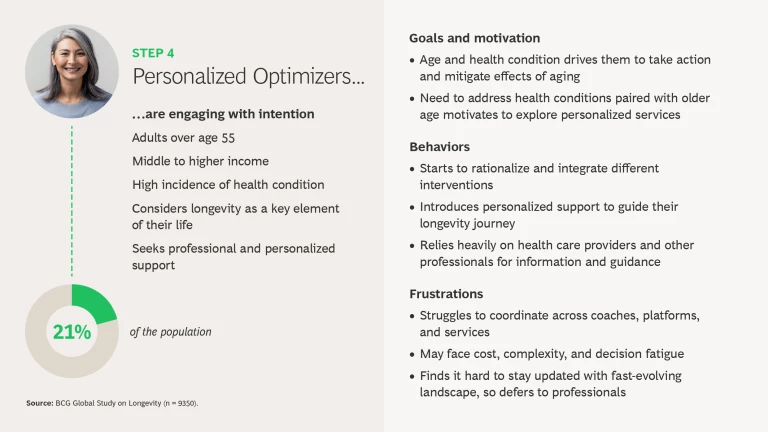
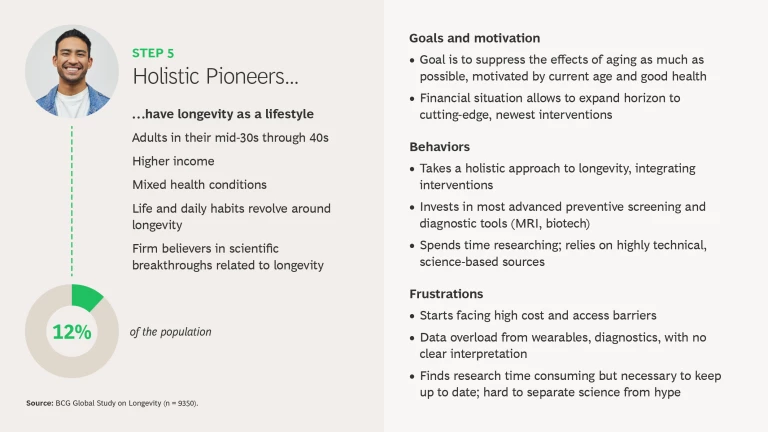
On the first rungs of the ladder, we find carefree Longevity Dismissers who just want to live life without worrying about healthy aging and the Longevity Curious who are intrigued but ultimately don’t take action. In the middle are Proactive Experimenters who are trying some things but struggle to make sense of what really works. On the top rungs of the ladder are the Personalized Optimizers who are taking more action and integrating their efforts and the Holistic Pioneers who are truly orienting their lifestyle around healthy aging and fully educating themselves on the scientific evidence. Note that many factors—not just age—impact people’s engagement with longevity behaviors. Younger people can be more engaged than older adults: each person has their own starting point.
Understanding Differences in Longevity Behaviors
What’s clear is that longevity engagement takes effort. Only 12% of respondents orient their lifestyle around healthy aging. What sets the most engaged people in our survey apart from the rest is a differentiated approach in both method and motivation. This group combines consumables, tech, services, and natural interventions to optimize their bodies and minds. Notably, they shift from reactive behaviors like taking vitamins to preventive and data-driven strategies, including cognitive apps, wearables, and advanced diagnostics.
Geographic differences also shape engagement patterns. People in emerging markets are more likely to use consumables and natural remedies, while developed markets lead in the usage of services, such as mental health therapies and advanced diagnostics. India, parts of Southeast Asia, and the Middle East stand out in terms of adopting wearables, apps, and tech solutions related to healthy aging, with 70% of respondents in these regions reporting usage. Longevity clinics are slowly making inroads, with particular growth in the Middle East, China, and Switzerland (with usage at double the global average in these countries).
Longevity resources and supports evolve in line with engagement. Less-engaged individuals learn through social networks, mass media, or passive content, while more-engaged individuals rely on evidence-based outlets such as scientific studies and targeted newsletters. Overall, there is still an important role for health care providers and pharmacies to influence decisions across all engagement stages, but younger generations in particular are bringing information they gather from influencers and social media (especially YouTube) into their discussions with doctors. Across generations and geographies, podcasts have emerged as a key influencer of perceptions and attitudes. Yet while over 80% of people are at least passively interested in longevity, only a third say they are taking any actions.
Longstanding Challenges to Personalized Health and Longevity Care
If health ambitions are personal, the systems designed to support them should be. But too often that’s not the experience for patients around the world.
Every individual’s needs are shaped by a unique combination of factors: age, physical and mental health, genetics, medical history, environment, access to caregivers, insurance coverage, and more. Yet despite this deeply personal nature, the health care system can feel anything but personalized.
There are several common pain points that will require action from multiple stakeholders working together to solve. Clinicians face more cost pressures and less time with patients among workforce shortages. Wait times for specialists and elective procedures continue to grow in many countries. Hospitals are discharging patients earlier, expecting families and home-based supports to fill the gaps in care. New medical technologies and treatments often push costs higher, not lower. Electronic health records remain fragmented and siloed.
So how do we help more people become more engaged with healthy aging behaviors—and start earlier in life—in a system that isn’t built for it? We begin by understanding each individual’s health ambitions and underlying motivations. Our survey results confirm the importance of health care providers in guiding people up the rungs of the Longevity Engagement Ladder. They remain the most trusted source of information across the five steps, even though primary care physicians in many countries lack the time or training to focus sufficiently on long-term goals like healthy aging.
Entering A New Era of Personalized Care
To address these many challenges, new forms of support are emerging. A growing class of AI-powered solutions act as personal health agents, helping people translate ambition into daily, actionable steps. For example, Noom uses AI-driven personalization to help individuals achieve weight loss and sustainable behavior change in areas like exercise. Sondermind, a mental health app in the US, starts off users with gamified exercises that measure 12 different brain functions to make personalized recommendations for therapists and measurement-based care. Ovum is an Australian AI health ally for women, a personal concierge that integrates user health history, medical reports, wearable data, and symptom tracking via conversational AI.
Our survey shows that such AI adoption is growing fastest in digitally forward markets like India (25% usage among local respondents), Indonesia (25%), and China (20%), where consumers are less constrained by privacy concerns. These tools are also gaining traction in some Western countries, such as Switzerland (14%) and Germany (10%).
What makes these solutions promising is their ability to work with an individual’s goals and translate progress into gamified and encouraging messages and incentives. Next-best-action suggestions in conversational language are easier for a person to embrace and act upon than generic health advice. As agentic AI technology advances, health care resources, information, and data can also be seamlessly integrated, avoiding bottlenecks and silos that can delay or limit patient care.
With the digitization of health care, lab results now reach patients instantly, and a new class of highly personalized diagnostic tools is emerging. Vitract, for example, offers rapid and easy gut microbiome analysis across a broad spectrum of biomarkers. Eternami offers AI-powered longitudinal health diagnostics and planning tailored to users’ biometric data. The health platform Fountain combines comprehensive lab testing with AI-powered scans to provide insights that help individuals understand their bodies and identify potential health issues early.
Tech-Enabled Personalized Health Requires Trust
An unforeseen consequence of these tools, however, is that people often get information and see test results before they’ve had a chance to talk to their provider or clinician. As noted earlier, people are turning to a wider set of sources for health information than ever before. To curtail the use of unreliable sources, it’s critical that digital solutions give people easy-to-understand information about their health, clearly explain what their test results mean, and instill a sense of control by explaining their options. (See “Report: The Path to Better Healthcare.”) Research shows that when patients feel in control and empowered to understand and navigate their care, adherence to treatment improves and recovery times accelerate.
Addressing this requires rethinking current approaches to data and privacy. Our 2025 study on personalization found that 80% of people would share personal information in exchange for a personalized experience, even in a health care setting.
Consumer trust is critical if AI-driven health tools are to help people pursue their health ambitions. History shows how quickly trust can be eroded by security breaches, data leaks, and unethical actions, such as health apps selling user information on data exchanges. Such incidents have prompted tighter regulations. The General Data Protection Regulation and privacy rules in the EU give consumers more control of how their data is used, but make it extremely difficult for researchers to conduct studies to understand health patterns and effective interventions.
Privacy and security will remain a challenge, but new capabilities—from data masking to decentralized management—can strengthen trust. Just as important, AI-driven recommendations must prioritize both a person’s health and their budget, rather than just promoting the most profitable options. This is especially true given our survey’s finding that lower-income segments have the most difficulty engaging in longevity behaviors.
The Path Forward
The five-step Longevity Engagement Ladder offers a roadmap and an opportunity for innovation. As consumer understanding of healthy aging deepens, their demands move beyond surface-level wellness toward personalized, proactive, and scientific longevity. For entrepreneurs, health care providers, and technologists, the takeaway is clear: longevity is no longer niche—it’s a growing ecosystem of informed, motivated individuals striving not just to live longer, but to live better.
The coming decade gives us great hope for the future of longevity. But we have a lot of work to do. Given the endless individual differences in people’s awareness, attitudes, and behavior and influence pathways, a personalized approach to longevity education and intervention is essential. The volume of content and channels to access this information is exploding, especially in a generative AI world, leaving most consumers overwhelmed. Right now, the healthy-aging economy—spanning supplements and consumables, services, wearables, and longevity centers—is vibrant and growing. But it’s also very disconnected and mixed in terms of its success in engaging people at the scale society needs.
The people who are fully engaged in their longevity journey offer a glimpse of what’s possible. They take daily action, seek out trusted information, and build out personalized routines that work for them. The challenge now is to scale this approach and build systems that support it. Doing so will require both individual change and collective action. Companies, governments, and stakeholders across health care systems all have a role to play in building more integrated, human-centered models of care.
Advances in AI, personalization, medical treatments, and accumulated learning will create new breakthroughs. But the race to bring them together into compelling, scalable models that engage healthy aging communities has just begun. It will take technology, human-centered design, empathy, and the ability to meet people where they are. Are you ready?